The 3D bioprinting of functional tissues is a complex, step-by-step process that depends on the designer. Now, however, biomedical engineers at Utrecht University have developed new technology published in Nature that integrates advanced imaging and artificial intelligence, enabling the 3D bioprinter to observe and analyse.
There is a shortage of life-saving organ donors. To address this issue, researchers are working on 3D-bioprinting organs (or parts of organs) that can perform certain bodily functions. The major challenge is keeping the cells in the printed tissue alive and ensuring they have the correct functionality. 3D bioprinters use a bioink for this purpose — typically a hydrogel containing cells and substances that the body accepts. By hardening the gel into the desired structure, the cells are fixed in place. However, determining the location of each layer and then connecting it to subsequent layers of tissue requires a great deal of complex manual work.
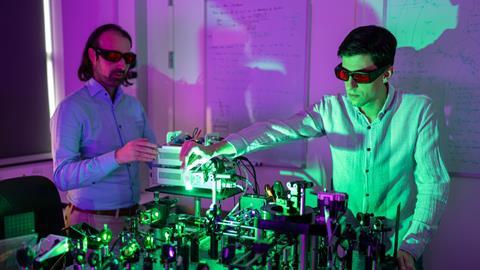
Researchers at Utrecht University have now developed a new method that enables 3D bioprinters to observe the printing process step by step. PhD student Sammy Florczak developed the technique, called Generative, Adaptive, Context-Aware 3D Printing (GRACE). GRACE uses lasers and artificial intelligence (AI) to identify the location of the cells in the printed ink. Riccardo Levato, a biomedical engineer from Utrecht University, led the research: ‘GRACE takes some of the work off our hands by generating designs that are better than we could come up with ourselves.’
Optimal blood vessels
While traditional 3D printers often print layer by layer, Levato and his team use volumetric bioprinting. This technique enables researchers to construct entire structures in seconds. They achieve this by projecting a series of 2D light patterns onto a rotating tube containing cells suspended in light-sensitive gel. Wherever the light converges, the gel hardens and fixes the cells in place. The result is 3D mini-tissues.
One of the biggest challenges in 3D bioprinting is accurately printing blood vessels. These are necessary for transporting oxygen and nutrients to the cells. However, current printing methods use a predetermined 3D design, making the correct placement of blood vessels difficult. ‘It remains unclear where exactly the cells will end up in the gel’, says Levato. ‘As a result, some cells end up far from the blood vessels and others close by.’ GRACE can determine the location of the cells and then design blood vessels so that all cells are no more than 200 micrometres from a blood vessel, ensuring they receive sufficient oxygen and nutrients.’
The technology can also connect multiple printing steps. For instance, GRACE can scan the surface of a printed piece of bone tissue and print a perfectly fitting layer of cartilage over it. It can also recognise opaque structures that do not allow light to pass through, generating a design that takes this into account. Levato explains, ‘We used GRACE to print cells through a stent, for example. Stents are porous, opaque tubes used in heart surgery.’
Virtual map
The bioprinter ‘sees’ using light sheet imaging. Levato explains, ‘We scan the rotating tube filled with bioink by shining a thin plane of light through it. This allows the printer to create a virtual map of everything in the tube.’ By making the cells fluorescent, GRACE can use the light beam to detect exactly where the cells are located.
The researchers demonstrated the considerable advantages of this virtual map by printing pancreatic cells alongside surrounding blood vessels. First, they had GRACE design and print an optimised network of blood vessels. Then, they compared this with a randomly printed network that had a similar surface area and diffusion properties. The result? The pancreatic cells in the optimised network produced more insulin. Levato: ‘That is exactly what such a printed structure is intended for.’
Smart baby
The researchers’ next step is to improve the resolution to make individual cells visible. ‘Currently, our technique has a resolution of 14 micrometres, which means we can only recognise groups of cells.’
The researchers also hope to make GRACE autonomous. Although the technique already uses some AI algorithms, it does not yet involve machine learning. ‘In this study, we had to provide GRACE with rules, such as the required distance between cells and blood vessels, and the desired number of blood vessel ends. Now, we want to enable the technique to learn from different networks, but this will require substantial data and training. In that respect, GRACE is still a smart baby, which we want to turn into a smart adult.’












Nog geen opmerkingen